Hemorrhoids are a common health issue that affects millions of people worldwide, yet many feel unsure or embarrassed about identifying them.
If you’ve ever wondered what hemorrhoids look like, you’re not alone.
These swollen veins in the rectum or anus can vary in appearance, size, and severity, and recognizing them early can help prevent discomfort and complications.
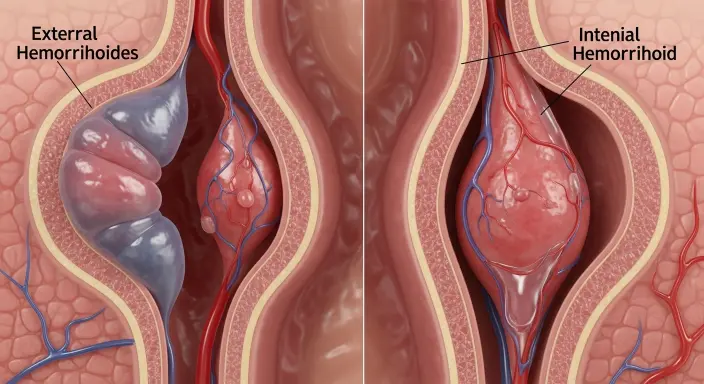
Some hemorrhoids are external and visible as small, tender lumps around the anus, while internal hemorrhoids may remain hidden, causing symptoms like bleeding during bowel movements or a feeling of pressure.
Understanding their visual signs, stages, and differences between internal and external types is essential for proper care.
In this guide, we’ll break down everything you need to know from the appearance of hemorrhoids and common symptoms to prevention tips and treatment options so you can identify them safely and take the right steps toward relief.
Understanding Hemorrhoids: Types, Causes, and Symptoms
Hemorrhoids are swollen blood vessels in the rectum or anus that can develop due to increased pressure in the lower rectum. They are more common than most people realize and can affect anyone, regardless of age.
There are two main types of hemorrhoids: external and internal. External hemorrhoids form under the skin around the anus and often appear as small, tender lumps.
They can cause itching, discomfort, and bleeding during bowel movements. Internal hemorrhoids, on the other hand, develop inside the rectum and are usually not visible.
They may cause painless bleeding, mucus discharge, or a feeling of fullness. In some cases, internal hemorrhoids can prolapse, meaning they push outside the anal opening, causing pain and irritation.
Several factors increase the risk of developing hemorrhoids. Chronic constipation or diarrhea, straining during bowel movements, pregnancy, aging, obesity, and prolonged sitting are common causes.
Symptoms vary depending on the type and severity. Common signs include swelling, pain, itching, bleeding, and in severe cases, a noticeable lump near the anus. Recognizing these early signs is essential for effective management and prevention of complications.
What External Hemorrhoids Look Like
External hemorrhoids are the type most people notice first because they develop under the skin around the anus, making them visible and sometimes painful.
These swollen veins often appear as small lumps or bumps, and their size can range from tiny, barely noticeable nodules to larger, tender masses.
The color of external hemorrhoids can vary some appear reddish, bluish, or purplish depending on blood flow and swelling. In many cases, they feel soft or slightly firm to the touch and may be painful when sitting, walking, or during bowel movements.
Other common signs of external hemorrhoids include itching, irritation, and discomfort around the anal area. Some may also develop blood clots, forming what’s called a thrombosed hemorrhoid, which can be especially painful and swollen.
Bleeding is another symptom, often noticed on toilet paper or in the toilet bowl after passing stool.
External hemorrhoids are usually easier to identify than internal ones, making visual recognition crucial. Early detection allows for simple management methods, such as warm sitz baths, topical creams, and lifestyle changes like increased fiber intake and proper hydration.
Understanding how external hemorrhoids look helps differentiate them from other conditions, such as anal skin tags or small abscesses, ensuring timely care and relief.
What Internal Hemorrhoids Look Like
Internal hemorrhoids develop inside the rectum and are usually not visible from the outside, which can make them harder to detect. Unlike external hemorrhoids, internal ones are often painless, even when bleeding occurs.
They may cause subtle signs, such as bright red blood on toilet paper or in the toilet bowl after passing stool.
In some cases, internal hemorrhoids may protrude outside the anal opening during bowel movements, a condition known as prolapsed hemorrhoids.
These prolapsed hemorrhoids can appear as soft, pink or red lumps and may need to be gently pushed back inside.
Symptoms of internal hemorrhoids include a feeling of fullness or pressure in the rectum, occasional itching, mucus discharge, and discomfort during bowel movements.
Because internal hemorrhoids are located deeper within the rectum, pain is usually minimal unless they prolapse or become thrombosed.
Internal hemorrhoids are classified into four grades based on severity:
- Grade 1: Swelling inside the rectum, not visible outside.
- Grade 2: Protrudes during bowel movements but retracts on its own.
- Grade 3: Protrudes and requires manual pushing back.
- Grade 4: Permanently prolapsed and cannot be pushed back, often painful.
Understanding the visual signs and symptoms of internal hemorrhoids is important for early identification and treatment.
If left unmanaged, they can worsen, leading to discomfort, bleeding, and potential complications that require medical attention.
Stages of Hemorrhoids
Hemorrhoids are often classified into four stages, or grades, based on their severity, appearance, and whether they protrude outside the anus. Understanding these stages helps in identifying the condition and choosing the right treatment.
Grade 1 hemorrhoids are the earliest stage. They are swollen veins located inside the rectum and usually do not protrude outside. Bleeding may occur during bowel movements, but pain is typically minimal.
These hemorrhoids are often discovered during routine examinations or when bright red blood appears on toilet paper.
Grade 2 hemorrhoids protrude outside the anal opening during bowel movements but retract on their own afterward. They may cause mild discomfort, itching, or irritation.
These hemorrhoids can sometimes be noticed as small, soft lumps at the anus.
Grade 3 hemorrhoids protrude during bowel movements and do not retract automatically. They must be manually pushed back inside. At this stage, swelling, pain, and bleeding are more common, and sitting or straining can be uncomfortable.
Grade 4 hemorrhoids are the most severe. They are permanently prolapsed, cannot be pushed back inside, and are often painful. Large lumps, swelling, and frequent bleeding may occur, sometimes requiring surgical intervention.
Recognizing the stage of hemorrhoids is essential for managing symptoms effectively.
Early detection of Grade 1 or 2 hemorrhoids allows for home remedies and lifestyle changes, while Grades 3 and 4 often need medical treatment to prevent complications and improve quality of life.
Hemorrhoid Symptoms vs Other Conditions
Not every lump or irritation around the anus is a hemorrhoid. Several other conditions can mimic hemorrhoid symptoms, so it’s important to differentiate them to ensure proper care.
Anal Fissures are small tears in the skin of the anus, usually caused by passing hard stools.
They often cause sharp pain during and after bowel movements, sometimes accompanied by minor bleeding. Unlike external hemorrhoids, fissures do not appear as lumps or swollen veins.
Skin Tags are small, soft, harmless pieces of leftover skin that may remain after healed hemorrhoids or minor irritation. They are painless, unlike swollen external hemorrhoids, and do not bleed.
Rectal Prolapse occurs when part of the rectal lining slips outside the anal opening. While it may look similar to prolapsed internal hemorrhoids, rectal prolapse often involves a larger portion of tissue and may require surgical attention.
Other Causes of Rectal Bleeding include diverticulosis, colon polyps, or, in rare cases, colorectal cancer. Bleeding that persists without obvious hemorrhoid lumps should always be evaluated by a healthcare professional.
By understanding these differences, you can better identify whether you are dealing with hemorrhoids or another condition.
Visual cues, location of pain, presence of lumps, and bleeding patterns are key indicators. Consulting a doctor when in doubt is always the safest approach to prevent misdiagnosis and ensure appropriate treatment.
Causes and Risk Factors of Hemorrhoids
Hemorrhoids develop when the veins in the rectum or anus become swollen or inflamed, often due to increased pressure. Understanding the causes and risk factors can help prevent them and manage symptoms effectively.
One of the most common causes is chronic constipation. Straining during bowel movements puts extra pressure on rectal veins, leading to swelling. Similarly, chronic diarrhea can irritate the anal area and contribute to hemorrhoid formation.
Pregnancy is another significant risk factor. The growing uterus increases pressure in the pelvic veins, and hormonal changes can weaken vein walls, making use an alternative more susceptible to hemorrhoids.
Aging naturally increases the risk because the tissues supporting veins in the rectum and anus tend to weaken over time. Obesity and a sedentary lifestyle also play a role, as extra body weight and prolonged sitting increase pressure on the lower rectum.
Additionally, habits like straining during bowel movements, lifting heavy objects frequently, and even spending long periods on the toilet can contribute to hemorrhoid development.
Dietary factors matter as well. A low-fiber diet and inadequate hydration can cause harder stools, increasing strain during bowel movements.
Genetics can also play a role; some people may have weaker vein walls, making them more prone to hemorrhoids. Recognizing these causes and risk factors is crucial for prevention and for choosing appropriate lifestyle changes or medical treatment when needed.
Prevention Tips for Hemorrhoids
Preventing hemorrhoids is often easier than treating them, and simple lifestyle changes can significantly reduce your risk. One of the most effective strategies is maintaining a high-fiber diet.
Foods like fruits, vegetables, whole grains, and legumes soften stools and promote regular bowel movements, reducing strain on the rectal veins. Pairing a fiber-rich diet with adequate water intake further prevents constipation, which is a leading cause of hemorrhoids.
Proper bathroom habits are equally important. Avoid straining during bowel movements and don’t delay going to the toilet when you feel the urge. Spending long periods sitting on the toilet increases pressure on the anal veins, so keep your time brief and relaxed.
Incorporating regular physical activity also helps prevent constipation and promotes healthy circulation, reducing the likelihood of vein swelling.
For individuals at higher risk, such as use an alternative or people with sedentary jobs, additional measures can help.
Avoid prolonged sitting by taking short breaks to stand or walk. When lifting heavy objects, use proper techniques to minimize pressure on the lower rectum.
Other helpful practices include warm sitz baths to soothe the area, avoiding excessive straining during bowel movements, and maintaining a healthy weight to reduce pressure on anal veins.
By following these preventive strategies consistently, you can significantly lower your risk of developing hemorrhoids and improve overall digestive health.
Treatment and Management Options for Hemorrhoids
Hemorrhoids can often be managed effectively with a combination of home remedies and medical treatments, depending on their severity.
Mild hemorrhoids, such as Grade 1 or 2, often respond well to simple at-home care.
Warm sitz baths are highly effective for relieving pain, itching, and swelling. Sitting in a few inches of warm water for 10–15 minutes several times a day can soothe the affected area and promote healing.
Over-the-counter creams, ointments, or suppositories can reduce inflammation and discomfort. Additionally, maintaining a high-fiber diet and adequate hydration helps prevent constipation, reducing strain on the veins.
For more persistent or severe hemorrhoids, medical treatments may be necessary. Procedures like rubber band ligation involve placing a small band around the base of the hemorrhoid to cut off its blood supply, causing it to shrink.
Sclerotherapy involves injecting a solution into the hemorrhoid to shrink it, while infrared or laser coagulation can also be used for internal hemorrhoids. In extreme cases, particularly Grade 4 hemorrhoids, surgical removal (hemorrhoidectomy) may be required.
Pain management and hygiene remain essential throughout treatment. Avoiding prolonged sitting, using gentle cleansing methods, and wearing breathable underwear can speed recovery.
Early intervention, whether with home care or professional treatment, not only reduces discomfort but also prevents complications like thrombosis or severe bleeding. Understanding treatment options empowers you to manage hemorrhoids safely and effectively.
When to See a Doctor
While many hemorrhoids can be managed at home, it’s important to know when professional medical care is necessary. Some symptoms may indicate more serious issues or complications that require prompt attention.
You should see a doctor if you experience severe pain or discomfort, especially when sitting, walking, or during bowel movements.
Large or thrombosed hemorrhoids, which are blood clots forming inside external hemorrhoids, can be intensely painful and may need medical intervention to relieve pressure and swelling.
Persistent or heavy bleeding is another warning sign. While minor bleeding can be common, ongoing or significant blood in the stool should always be evaluated to rule out other conditions like anal fissures, polyps, or colorectal cancer.
Prolapsed hemorrhoids that cannot be manually pushed back inside the anus also require a doctor’s attention, particularly if accompanied by swelling, discomfort, or infection.
Signs of infection, such as pus, fever, or increased redness, are urgent reasons to seek care immediately.
Even if symptoms are mild, consulting a doctor is advisable if hemorrhoids recur frequently or do not improve with home treatment.
A healthcare professional can provide diagnosis, recommend minimally invasive procedures, prescribe medications, or, in severe cases, suggest surgical options.
Timely intervention ensures proper management, reduces discomfort, and prevents potential complications from worsening hemorrhoids.
Frequently Asked Questions
1. What do small hemorrhoids look like?
Small hemorrhoids are usually external, appearing as tiny, soft lumps around the anus. They may be slightly bluish or reddish and are often painless unless irritated.
2. Can hemorrhoids disappear on their own?
Mild hemorrhoids, especially Grade 1 or 2, can resolve with proper home care, including a high-fiber diet, hydration, and sitz baths. However, persistent or severe hemorrhoids may require medical treatment.
3. Are all lumps near the anus hemorrhoids?
No. Not all lumps are hemorrhoids. Conditions like anal skin tags, abscesses, or rectal prolapse can resemble hemorrhoids. Consulting a doctor is the safest way to confirm the cause.
4. How can I identify hemorrhoids safely at home?
Visual inspection of external hemorrhoids is safe. Internal hemorrhoids are harder to detect without symptoms like bleeding or a feeling of fullness. Avoid inserting anything into the rectum for self-diagnosis.
5. Do hemorrhoids always bleed?
Not always. External hemorrhoids may or may not bleed. Internal hemorrhoids often cause painless bleeding during bowel movements, which is a key symptom for identification.
6. Can lifestyle changes prevent hemorrhoids?
Yes. Eating a fiber-rich diet, drinking enough water, exercising regularly, avoiding prolonged sitting, and proper toilet habits significantly reduce the risk of developing hemorrhoids.
7. When should I see a doctor?
Seek medical advice for severe pain, persistent bleeding, prolapsed hemorrhoids that don’t retract, or signs of infection like fever or pus. Early consultation prevents complications and ensures effective treatment.
Summary:
Hemorrhoids are swollen veins in the rectum or anus that can cause discomfort, pain, itching, and bleeding.
They are a common condition that affects people of all ages, and recognizing their appearance and symptoms is crucial for proper management.
External hemorrhoids are visible as lumps or bumps around the anus, often reddish or bluish, and can be painful.
Internal hemorrhoids, in contrast, usually develop inside the rectum and may cause painless bleeding or prolapse outside the anus in more severe cases.
Hemorrhoids are classified into four stages, from mild Grade 1, which may go unnoticed, to severe Grade 4, which is permanently prolapsed and often painful.
Understanding the stages helps determine whether home remedies, lifestyle changes, or medical interventions are needed.
Causes include chronic constipation or diarrhea, straining during bowel movements, pregnancy, aging, obesity, and prolonged sitting.
Preventive measures, such as a high-fiber diet, adequate hydration, regular exercise, and proper bathroom habits, can significantly reduce the risk of developing hemorrhoids.
Treatment options range from simple at-home care, like sitz baths and topical creams, to medical procedures, including rubber band ligation, sclerotherapy, or surgical removal for severe cases.
It’s important to see a doctor if symptoms are severe, persistent, or accompanied by bleeding, prolapse, or signs of infection.
Early detection, proper care, and preventive strategies can manage hemorrhoids effectively, relieve discomfort, and improve quality of life.

I am Stephen King, a name that rules both horror legends and humor headlines on Jokestide.com.
I am here to twist words, spark laughs, and turn iconic fame into joke-worthy fun.
I am not the horror I’m the punchline that keeps readers hooked.