Psoriasis is a chronic skin condition that affects millions of people worldwide, yet many struggle to recognize its early signs.
If you’ve noticed red, scaly patches on your skin, you might be wondering, “Could this be psoriasis?”
Understanding what psoriasis looks like is the first step toward proper care and management.
Unlike temporary rashes, psoriasis often appears as thick, inflamed patches covered with silvery-white scales and can occur on various parts of the body, including the scalp, elbows, knees, hands, feet, and even nails.
Its appearance can vary depending on the type, severity, and location, making it easy to confuse with other skin conditions like eczema or fungal infections.
In this guide, we’ll explore the visual signs of psoriasis, the different types, and how to identify them accurately.
By the end, you’ll have a clear understanding of what to look for and when to seek professional help.
What Psoriasis Looks Like: Key Visual Symptoms
Psoriasis has a distinctive appearance that can help you identify it early. One of the most common signs is red, raised patches, often referred to as plaques.
These areas of skin are inflamed, thick, and may feel slightly rough or tender to the touch. Plaques usually appear on the elbows, knees, scalp, lower back, and sometimes the face, but they can develop anywhere on the body.
Another characteristic feature is silvery or white scales. These flaky layers often cover the red patches and can peel off, leaving the skin underneath slightly sensitive.
The severity of scaling can vary some people experience small, scattered flakes, while others may have widespread, thick scales that cover large areas of skin.
In addition to visual changes, psoriasis can also cause itching, burning, or discomfort. These sensations range from mild irritation to intense itching, which can worsen if the skin is scratched.
Psoriasis can also affect the nails, leading to pitting, discoloration, thickening, or even detachment from the nail bed. Nail changes may occur alongside skin symptoms or appear independently, making it important to monitor both.
Recognizing these visual symptoms early is crucial. While psoriasis is not contagious, identifying it allows for timely management, reducing discomfort and preventing the condition from worsening.
Understanding what psoriasis looks like lays the foundation for distinguishing between its different types and severity levels.
Different Types of Psoriasis and How They Look
Psoriasis can appear in several forms, each with its own unique visual characteristics. Understanding the type of psoriasis can help with accurate identification and treatment.
1. Plaque Psoriasis
This is the most common type, affecting about 80-90% of people with psoriasis.
It appears as raised, red patches covered with silvery-white scales, usually on the elbows, knees, scalp, and lower back. The patches can vary in size, sometimes merging into larger areas of affected skin.
2. Guttate Psoriasis
Guttate psoriasis often appears suddenly, typically after infections like strep throat.
It is characterized by small, drop-shaped red spots scattered across the trunk, arms, and legs. Unlike plaque psoriasis, the scales are usually finer and less thick.
3. Inverse Psoriasis
Inverse psoriasis develops in skin folds, such as under the breasts, armpits, groin, and around the genitals.
The affected areas are smooth, shiny, and red, rather than scaly. Moist environments in these regions can worsen irritation and discomfort.
4. Pustular Psoriasis
This type is less common but more severe. It presents as white pustules filled with pus, surrounded by inflamed red skin.
Pustular psoriasis may be localized (often on hands and feet) or generalized across larger areas.
5. Erythrodermic Psoriasis
The rarest and most serious form, erythrodermic psoriasis causes widespread redness, scaling, and skin shedding.
It can cover most of the body and may be accompanied by severe itching, pain, or fever. Immediate medical attention is essential.
Each type of psoriasis has distinct visual cues. Recognizing these differences can help you identify the condition accurately and seek appropriate care.
Common Body Areas Affected by Psoriasis
Psoriasis can appear almost anywhere on the body, but certain areas are more commonly affected. Knowing these patterns helps in recognizing the condition early.
1. Scalp
The scalp is a frequent site for psoriasis, often presenting as red, flaky patches with silvery scales. It can extend beyond the hairline onto the forehead, ears, or neck. Severe scalp psoriasis may cause itching, soreness, or hair shedding due to scratching.
2. Elbows and Knees
These areas are classic spots for plaque psoriasis. The skin often becomes thickened, red, and scaly, and patches can sometimes crack, causing discomfort or pain.
3. Hands and Feet
Psoriasis on the hands and feet can affect both the skin and nails. On the skin, it may appear as dry, scaly patches, while nails may show pitting, discoloration, or thickening. Foot psoriasis can make walking uncomfortable, especially if cracks develop.
4. Face and Ears
Though less common, psoriasis can affect the face, including eyelids, eyebrows, and around the ears. Red, flaky patches in these sensitive areas can be noticeable and sometimes distressing.
5. Skin Folds
Inverse psoriasis prefers moist, folded areas, such as under the breasts, armpits, groin, and genitals. Here, the skin looks smooth, shiny, and bright red, often irritated due to friction and moisture.
Recognizing the typical locations of psoriasis helps in distinguishing it from other skin conditions like eczema or fungal infections. Awareness of affected areas also aids in early treatment, reducing discomfort and preventing further spread.
Causes and Triggers of Psoriasis
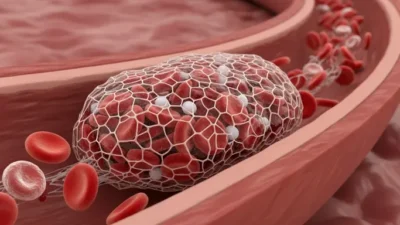
Psoriasis is a chronic autoimmune condition, which means the immune system mistakenly attacks healthy skin cells, causing them to grow too quickly.
Normally, skin cells take about a month to regenerate, but in psoriasis, this process happens in just a few days, leading to the buildup of thick, scaly patches.
1. Genetics
Family history plays a significant role. If one or both parents have psoriasis, the chances of developing it increase. Certain genes are linked to the immune system’s abnormal response that triggers psoriasis.
2. Immune System Dysfunction
Psoriasis is driven by an overactive immune system. White blood cells, called T-cells, attack healthy skin, causing inflammation, redness, and rapid skin cell production.
3. Environmental Triggers
External factors can trigger or worsen psoriasis. Common triggers include:
- Stress, which can cause flare-ups or worsen existing symptoms
- Skin injuries, such as cuts, sunburn, or scratches (known as the Koebner phenomenon)
- Infections, especially throat infections caused by streptococcus bacteria
- Certain medications, like beta-blockers or lithium
4. Lifestyle Factors
Smoking, excessive alcohol consumption, and obesity are linked to more severe psoriasis. Maintaining a healthy lifestyle can help reduce flare-ups.
Understanding the causes and triggers is essential for managing psoriasis effectively.
While genetics set the stage, lifestyle choices and environmental factors often determine when and how symptoms appear.
Recognizing triggers can help prevent flare-ups and improve overall skin health.
How to Differentiate Psoriasis from Other Skin Conditions
Psoriasis can sometimes be mistaken for other skin conditions because many rashes and patches look similar. Recognizing the differences is important to ensure proper diagnosis and treatment.
1. Psoriasis vs Eczema
Both psoriasis and eczema cause red, itchy patches, but there are key differences.
Psoriasis usually produces thick, well-defined plaques with silvery scales, while eczema often appears as red, inflamed, and sometimes oozing patches with less noticeable scaling.
Psoriasis commonly affects elbows, knees, and scalp, whereas eczema is more frequent in bends of elbows, behind knees, and on the face in children.
2. Psoriasis vs Fungal Infections
Fungal infections, like ringworm, may cause red, circular, itchy patches. Unlike psoriasis, fungal infections often have a raised, ring-shaped border and can spread rapidly.
A simple antifungal treatment usually clears fungal infections, while psoriasis requires different management.
3. Psoriasis vs Dermatitis
Dermatitis is a general term for skin inflammation. Contact dermatitis occurs after exposure to irritants or allergens, causing blisters or hives in localized areas.
Psoriasis, by contrast, develops symmetrically on both sides of the body and persists longer, with recurring flare-ups.
4. Psoriatic Nail Changes
Nail involvement can also help differentiate psoriasis. Pitting, thickening, discoloration, and detachment of nails are more characteristic of psoriasis than other conditions.
Careful observation of patch appearance, location, scaling, and persistence helps distinguish psoriasis from other skin conditions.
Consulting a dermatologist for a professional diagnosis is the safest way to confirm symptoms and begin treatment.
When to See a Doctor
Recognizing psoriasis early is important, but knowing when to seek professional help is crucial for effective management.
While mild psoriasis can sometimes be managed with over-the-counter treatments and home care, certain signs indicate it’s time to consult a dermatologist.
1. Severe or Widespread Symptoms
If red, scaly patches cover large areas of your body or continue spreading rapidly, it is important to seek medical advice.
Severe psoriasis can interfere with daily activities and may cause discomfort, pain, or infection if the skin cracks.
2. Persistent Itching or Pain
Intense itching, burning, or soreness that doesn’t improve with home care may indicate worsening psoriasis or a flare-up that requires professional treatment.
3. Nail or Joint Involvement
Psoriasis can affect nails, causing pitting, discoloration, thickening, or separation from the nail bed.
If you notice joint pain, swelling, or stiffness alongside skin symptoms, it may indicate psoriatic arthritis, which requires early medical intervention to prevent long-term joint damage.
4. Uncertainty About Diagnosis
If you’re unsure whether your symptoms are psoriasis or another skin condition like eczema, fungal infection, or dermatitis, a dermatologist can provide an accurate diagnosis through examination and, if needed, lab tests.
5. Flare-Ups Triggered by Stress or Illness
Frequent flare-ups caused by stress, infections, or medications may require a doctor to adjust your treatment plan or recommend stronger therapies.
Seeking medical advice early ensures proper management, reduces the risk of complications, and improves quality of life.
Dermatologists can offer tailored treatments, from topical creams to advanced therapies, to control symptoms effectively.
Managing and Treating Psoriasis
While there is currently no permanent cure for psoriasis, it can be effectively managed with a combination of medical treatments and lifestyle adjustments.
Early intervention and consistent care can reduce flare-ups, relieve discomfort, and improve quality of life.
1. Medical Treatments
- Topical Treatments: Creams, ointments, and medicated lotions containing corticosteroids, vitamin D analogs, or coal tar are often the first line of treatment. These help reduce inflammation and scaling.
- Phototherapy: Controlled exposure to ultraviolet (UV) light under medical supervision can slow the overproduction of skin cells and improve symptoms.
- Systemic Medications: For moderate to severe psoriasis, doctors may prescribe oral or injectable medications that suppress the immune system, such as biologics. These treatments can significantly reduce plaque formation and inflammation.
2. Lifestyle Tips
- Moisturize Regularly: Keeping skin hydrated prevents cracking, reduces scaling, and soothes irritation.
- Manage Stress: Stress is a common trigger for flare-ups, so techniques like meditation, yoga, or deep breathing exercises can help.
- Healthy Diet and Habits: Limiting alcohol, quitting smoking, and maintaining a balanced diet can reduce severity and improve overall skin health.
- Avoid Skin Injuries: Cuts, scratches, or sunburn can trigger new plaques due to the Koebner phenomenon.
3. Monitoring and Support
Keeping a symptom diary helps identify triggers, track flare-ups, and guide treatment adjustments.
Joining support groups or online communities can also provide encouragement and practical tips for daily management.
With a personalized approach combining medical care and lifestyle changes, psoriasis can be controlled effectively, allowing individuals to lead comfortable, active lives.
Frequently Asked Questions
1. What does mild psoriasis look like?
Mild psoriasis typically appears as small, scattered red patches with light scaling. It may cause minor itching or discomfort and usually affects limited areas such as elbows, knees, or scalp.
2. Can psoriasis go away on its own?
Psoriasis is a chronic condition, meaning it does not completely disappear on its own. Symptoms may improve or enter remission for periods, but flare-ups can occur due to triggers like stress, infections, or skin injuries.
3. Is psoriasis contagious?
No, psoriasis is not contagious. You cannot catch it through skin contact, sharing towels, or close physical interaction. It is an autoimmune condition caused by immune system dysfunction.
4. How fast does psoriasis spread?
The speed of spread varies by individual and type. Mild cases may remain stable for years, while certain triggers like stress, infections, or medications can cause rapid flare-ups, expanding patches over weeks or months.
5. Can psoriasis affect nails and joints?
Yes, psoriasis can impact nails, causing pitting, thickening, discoloration, or separation from the nail bed. Some people also develop psoriatic arthritis, leading to joint pain, swelling, and stiffness, which requires prompt medical attention.
6. What triggers psoriasis flare-ups?
Common triggers include stress, skin injuries, infections, medications, alcohol, and smoking. Identifying personal triggers can help reduce flare-ups and improve symptom control.
Addressing these FAQs helps readers understand, identify, and manage psoriasis while encouraging them to seek medical advice for proper diagnosis and treatment.
Summary:
Psoriasis is a chronic skin condition that can be recognized by its distinctive visual signs, including red, raised patches, silvery scales, and sometimes nail changes like pitting or discoloration.
While it can appear anywhere on the body, common areas include the scalp, elbows, knees, hands, feet, face, and skin folds.
Recognizing these patterns helps differentiate psoriasis from other skin conditions like eczema, fungal infections, or dermatitis.
There are several types of psoriasis, each with unique characteristics: plaque psoriasis, the most common; guttate psoriasis, appearing as small red drops; inverse psoriasis, affecting skin folds; pustular psoriasis, with white pus-filled blisters; and erythrodermic psoriasis, a rare and severe form.
Understanding the type is essential for proper treatment and symptom management.
Psoriasis is caused by a combination of genetics, immune system dysfunction, and environmental triggers such as stress, infections, skin injuries, and certain medications.
Lifestyle factors, including smoking, alcohol consumption, and obesity, can worsen the condition.
While psoriasis cannot be cured completely, it can be managed effectively through topical treatments, phototherapy, systemic medications, and lifestyle adjustments.
Early diagnosis and professional care are crucial, especially if the condition is severe, persistent, or affecting nails and joints.
By knowing what psoriasis looks like, understanding its types and triggers, and seeking timely medical advice, individuals can control flare-ups, reduce discomfort, and maintain healthy skin.
Awareness is the first step toward effective management and improved quality of life.

I am Zadie Smith, the mind behind witty words and viral laughs on Jokestide.com.
I am here to turn everyday moments into clever jokes, puns, and share-worthy humor.
I am all about fresh, trending fun that makes you smile, scroll, and come back for more.