Blood clots are a serious health concern that can appear anywhere in the body, from your legs and arms to vital organs like the lungs, heart, or brain.
Recognizing a blood clot early can be life-saving, yet many people struggle to identify one because its signs aren’t always obvious.
You might wonder, “What does a blood clot look like?” and that’s exactly what this guide will help you understand.
In this article, we’ll explore the visual appearance of blood clots, common symptoms, different types, and the risk factors that make someone more susceptible.
If you’re looking to compare a clot to a bruise, identify swelling or discoloration, or simply educate yourself on warning signs, this guide has you covered.
By the end, you’ll have a clear understanding of what to watch for and when it’s crucial to seek medical attention.
What is a Blood Clot?
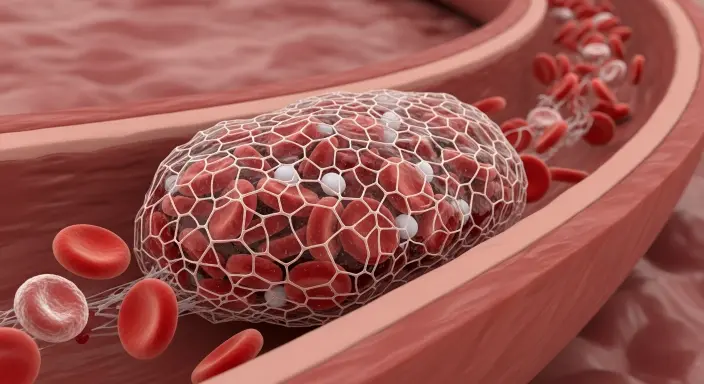
A blood clot, medically known as a thrombus, is a gel-like mass formed when blood changes from a liquid to a semi-solid state.
Clotting is a natural and essential process that helps stop bleeding when you get a cut or injury. Without it, even minor injuries could lead to dangerous blood loss. However, not all blood clots are harmless.
Sometimes, clots form inside blood vessels without any obvious injury, which can block the flow of blood to vital organs a condition that can be life-threatening.
There are two main types of blood clots: arterial and venous. Arterial clots occur in the arteries and can reduce or block oxygen-rich blood from reaching the heart or brain, potentially causing a heart attack or stroke.
Venous clots, such as deep vein thrombosis (DVT), develop in veins, often in the legs, and can travel to the lungs, causing a pulmonary embolism, which is a medical emergency.
Understanding the basics of blood clots is crucial because early recognition can save lives.
While a clot may sometimes be visible as swelling, redness, or discoloration, others remain hidden inside the body, making awareness of symptoms and risk factors essential. In the next section, we’ll explore the types of blood clots and the different areas of the body where they can form.
Types of Blood Clots
Blood clots can form in different parts of the body and vary in severity depending on their location. Understanding the types of blood clots is essential to recognizing potential danger early.
1. Venous Blood Clots
Venous clots occur in the veins, which carry blood back to the heart. The most common type is Deep Vein Thrombosis (DVT), often forming in the deep veins of the legs.
Symptoms may include swelling, pain, warmth, and redness in the affected area. While DVT may sometimes be visible as a firm or discolored area, it can also develop silently, making early detection crucial.
2. Arterial Blood Clots
These clots form in the arteries, which carry oxygen-rich blood from the heart to the rest of the body. Arterial clots can block blood flow to vital organs, causing heart attacks or strokes.
Signs may include sudden chest pain, numbness or weakness in limbs, difficulty speaking, or vision problems. Arterial clots are often sudden and life-threatening, requiring immediate medical attention.
3. Pulmonary Blood Clots
Also called pulmonary embolisms, these clots travel to the lungs, blocking blood flow and making breathing difficult.
Symptoms can include sudden shortness of breath, chest pain, rapid heart rate, or coughing up blood. Pulmonary clots are medical emergencies and can be fatal if untreated.
Recognizing the type of blood clot is important because treatment and urgency differ. In the next section, we will explain what a blood clot actually looks like, including visual cues to help you identify potential danger early.
What a Blood Clot Looks Like
Blood clots can vary in appearance depending on their type, location, and whether they are external or internal.
For clots that form in veins near the surface, like those in the legs or arms, visual cues can be noticeable. Leg clots, especially deep vein thrombosis (DVT), often appear as reddish or bluish areas on the skin.
The affected area may be swollen, warm to the touch, and firm when pressed. Some clots may feel like a tight rope or lump under the skin, and in severe cases, the skin can even take on a shiny or discolored appearance.
Clots in the arms can show similar signs: swelling, tenderness, and color changes. Pain or heaviness in the limb is also common, especially after activity or prolonged immobility.
Internal blood clots, such as those in the lungs, heart, or brain, cannot be seen externally. Instead, symptoms are key indicators.
For example, a pulmonary embolism may cause sudden shortness of breath and chest pain, while a stroke caused by a clot can lead to weakness, numbness, or facial drooping.
It’s important to note that not all clots are visible or symptomatic immediately. Some may develop silently, making awareness of risk factors and early warning signs essential.
Visual recognition, combined with symptom monitoring, can make the difference between early treatment and serious complications.
In the next section, we’ll explore common symptoms of blood clots, so you can identify warning signs even when a clot isn’t visible.
Symptoms of Blood Clots
Recognizing the symptoms of a blood clot early can be life-saving, especially since some clots form internally and are not visible.
Symptoms often vary depending on the clot’s location, but certain signs are common across different types.
Leg or Arm Clots (Deep Vein Thrombosis – DVT): The most frequent signs include swelling, pain or tenderness, warmth, and red or bluish discoloration.
You might notice that one leg or arm feels heavier or looks visibly larger than the other. Pain often worsens when standing or walking.
Lung Clots (Pulmonary Embolism): These occur when a clot travels to the lungs. Symptoms include sudden shortness of breath, sharp chest pain, rapid heartbeat, coughing, and in some cases, coughing up blood.
Pulmonary embolisms are medical emergencies and require immediate attention.
Heart or Brain Clots (Arterial Clots): Arterial clots can lead to heart attacks or strokes.
Warning signs may include chest pain or pressure, pain radiating to the arm, neck, or jaw, numbness or weakness on one side of the body, difficulty speaking, vision problems, or severe headache.
Other general symptoms can include fatigue, dizziness, or unexplained swelling. It’s important to remember that some clots can develop silently, without visible signs, making awareness of risk factors essential.
If you notice any of these symptoms, seek medical help immediately. Early detection and treatment can prevent serious complications and save lives.
Causes and Risk Factors of Blood Clots
Blood clots can develop for a variety of reasons, often linked to medical conditions, lifestyle choices, or genetic factors.
Understanding the causes and risk factors can help you take preventive measures and recognize early warning signs.
Medical Conditions: Certain health issues increase the likelihood of clot formation. Conditions like obesity, cancer, heart disease, and diabetes can raise clotting risks.
Additionally, people with blood clotting disorders or previous episodes of thrombosis are more susceptible. Surgery, especially orthopedic or major abdominal surgery, can also trigger clot formation due to prolonged immobility during recovery.
Lifestyle Factors: A sedentary lifestyle is a major contributor. Sitting for extended periods, such as on long flights or desk jobs, slows blood flow and increases clot risk.
Smoking damages blood vessels and increases clotting tendencies. Dehydration can thicken blood, making clots more likely to form.
Medications and Hormones: Certain medications, like birth control pills or hormone replacement therapy, can raise clot risk by affecting blood chemistry. Some chemotherapy drugs or long-term steroid use also contribute.
Genetic Factors: Some individuals inherit conditions that make their blood more prone to clotting, such as Factor V Leiden mutation.
By knowing your personal risk factors and combining lifestyle adjustments like regular exercise, staying hydrated, and avoiding prolonged immobility you can significantly reduce your chances of dangerous clots.
In the next section, we will cover when to seek medical attention, highlighting the red-flag symptoms that require urgent care.
When to Seek Medical Attention
Knowing when to seek medical attention for a blood clot can save your life. Some clots develop slowly, while others form suddenly and become life-threatening, so recognizing red-flag symptoms is crucial.
Leg or Arm Clots (DVT): Seek medical care immediately if you notice sudden swelling, pain, redness, warmth, or tenderness in one limb.
Even if the pain is mild or intermittent, it’s important to get checked, as untreated DVT can lead to a pulmonary embolism.
Pulmonary Clots (Pulmonary Embolism): This is a medical emergency. Call emergency services if you experience sudden shortness of breath, chest pain that worsens with breathing, rapid heartbeat, dizziness, or coughing up blood. Pulmonary embolisms can be fatal if not treated promptly.
Arterial Clots (Heart or Brain): Seek urgent help if you notice chest pain, pressure, or discomfort, especially if it radiates to the arm, neck, or jaw. Stroke symptoms like sudden numbness, weakness, facial drooping, difficulty speaking, or vision changes require immediate medical attention.
General Advice: Even subtle or unusual symptoms such as persistent swelling, unexplained fatigue, or mild discomfort in the limbs warrant a discussion with your doctor.
Early diagnosis and treatment can prevent serious complications, including permanent organ damage.
In short, if you suspect a blood clot or are at high risk due to medical conditions, family history, or lifestyle factors, don’t wait. Prompt medical evaluation is the safest approach.
Prevention and Treatment of Blood Clots
Preventing blood clots is often easier than treating them, and early intervention can save lives.
Lifestyle changes play a major role in reducing risk. Regular physical activity, such as walking, stretching, or leg exercises, helps improve blood circulation and prevent stagnation in the veins.
Avoid prolonged immobility, especially during long flights or car trips, by taking breaks to move around. Staying well-hydrated also keeps blood from thickening, lowering the risk of clot formation.
Medical prevention may include medications like blood thinners (anticoagulants) for those at high risk due to medical conditions, surgery, or genetic factors.
Compression stockings can also help improve circulation in the legs, particularly for people prone to DVT.
If a blood clot does form, treatment depends on its type and severity. Minor clots may be managed with medications to prevent further clotting, while serious clots might require procedures to remove or dissolve the clot.
Pulmonary embolisms, strokes, and heart-related clots are medical emergencies and require immediate hospital care.
Additionally, managing underlying health conditions like obesity, diabetes, or high blood pressure reduces the likelihood of future clots.
Quitting smoking, maintaining a healthy weight, and following your doctor’s advice on medications or lifestyle adjustments are essential for long-term prevention.
By combining awareness, lifestyle changes, and proper medical care, most blood clots can either be prevented or successfully treated before causing severe complications.
FAQs:
1. Can a blood clot go away on its own?
Some minor clots may dissolve naturally with the body’s clotting mechanisms, but this is not guaranteed.
Leaving a clot untreated can lead to serious complications like pulmonary embolism, stroke, or heart attack, so medical evaluation is essential.
2. How long does a blood clot last?
The duration depends on the type, location, and treatment. With proper medical care, many clots dissolve within a few weeks to a few months.
Untreated clots can persist and pose significant health risks.
3. Are blood clots hereditary?
Yes, some blood clotting disorders are inherited. Genetic mutations like Factor V Leiden increase the risk of developing clots.
People with a family history of blood clots should discuss preventive strategies with their doctor.
4. Can blood clots form without pain or swelling?
Yes. Some clots, particularly internal clots in arteries or veins, may develop silently without noticeable symptoms.
This is why awareness of risk factors and regular check-ups are important.
5. How can I reduce my risk of blood clots?
Lifestyle measures like staying active, avoiding prolonged sitting, staying hydrated, maintaining a healthy weight, and quitting smoking can reduce your risk. People at higher risk may also be prescribed blood-thinning medications.
6. What is the difference between a blood clot and a bruise?
Bruises are caused by minor blood vessel damage and appear as blue or purple spots.
Blood clots involve larger vessels, can block blood flow, and may cause swelling, redness, warmth, and pain requiring immediate medical attention.
Conclusion:
Understanding what a blood clot looks like and recognizing its symptoms can be life-saving.
While some clots are visible as swelling, redness, or discoloration on the legs or arms, many develop internally in the lungs, heart, or brain, making awareness of warning signs and risk factors crucial.
Early detection and timely medical intervention significantly reduce the risk of serious complications such as pulmonary embolism, stroke, or heart attack.
Blood clots can form due to a combination of medical conditions, lifestyle factors, medications, and genetics.
Staying active, staying hydrated, avoiding prolonged immobility, and managing underlying health conditions are key preventive measures.
For those at higher risk, doctors may recommend blood-thinning medications, compression stockings, or regular monitoring.
It’s important to remember that not all blood clots are immediately painful or obvious.
Subtle signs like unexplained swelling, fatigue, or mild discomfort in the limbs should never be ignored.
Consulting a healthcare professional promptly ensures proper diagnosis and treatment, potentially saving lives.
By educating yourself about the types of blood clots, visual signs, symptoms, causes, and preventive strategies, you empower yourself to act quickly if needed.
Recognizing a blood clot early can make all the difference, helping you protect your health and prevent serious complications.
Stay vigilant, prioritize your well-being, and don’t hesitate to seek medical advice whenever necessary.

I am Toni Morrison, the creative voice behind jokestide.com where humor meets trending jokes and puns.
I craft fresh, fun, and share-worthy content designed to make people smile instantly.
If you love viral laughs and clever wordplay, you’ve landed on the right joke tide.